Getting to the Root of Your Pain: How an MRI Can Help Diagnose Musculoskeletal Conditions
Musculoskeletal disorders are common but often severe conditions that affect muscles and tendons. In this article, we will explore what musculoskeletal disorders are, how people get them, and the ways MRIs diagnose and treat these ailments.

What Are Musculoskeletal Disorders?
Musculoskeletal disorders, or MSDs, are conditions that impact the musculoskeletal system. The musculoskeletal system is comprised of bones, ligaments, tendons, and muscles. The musculoskeletal system allows the human body to move. People who suffer from MSDs usually experience persistent pain that limits their mobility and dexterity. Common MSDs include:
- Tendonitis
- Carpal tunnel syndrome
- Ligament sprain
- Epicondylitis
- Thoracic outlet compression
- Mechanical back syndrome
- And many more
MSDs are the most common workplace injury. According to the U.S. Bureau of Labor Statistics, 30 percent of worker’s compensation costs derive from MSDs. More often than not, people develop MSDs not from a single traumatic incident, but from repeated stressors put on their bodies. Fittingly, other common names for this type of injury are “repetitive stress injury,” “overuse injury,” and “repetitive motion injury.” Anyone who has ever felt soreness after repeating the same task has some concept of an MSD, though the injuries we will explore in this article are far more severe than simple soreness.
How Do People Get Musculoskeletal Disorders
People often experience fatigue from their work tasks. Your neck might feel stiff after staring down all day, or you might feel a pain in your back from carrying bulky objects for many hours. But there’s a difference between normal fatigue and MSDs. MSDs develop when the body doesn’t have the time to recover before you apply more strain, compounding the pain. Too much persistent pressure eventually creates a musculoskeletal imbalance. People either experience these stress factors from activities forced upon them by their employers, which we call work-related risk factors, or from activities they decide to do themselves, which we call individual-related risk factors.
Work-Related Risk Factors
When an employee is made to complete tasks at work that exceed their body’s capabilities, they put their musculoskeletal system in danger. We call those tasks work-related risk factors. Nobody should ever be made to feel unsafe at work. Unfortunately, in this hyper-competitive job market, employers very often push workers far more than they should. We can break down work-related risk factors into three primary categories:
- High task repetition—People can form MSDs from repetitive tasks. Many jobs are repetitive. Think about the common image of assembly line workers screwing in bolts again and again throughout an entire day. Doing those same tasks all the time puts a strain on a person’s body. These high task repetitions over time may lead to an MSD.
- Forceful exertion—Whereas some jobs require the repetition of tasks that, when taken together, put too much strain on the body, some jobs may ask a person to complete one single task that
creates too much tension. Even lifting a heavy manhole once, for example, may be too much for a person’s back and may permanently damage their spine. That is an example of forceful exertion.
- Repetitive or sustained awkward postures—Joints are not meant to remain in an awkward position for too long. If your job asks you to stand or sit in an awkward position all day, and you feel pain as a result, you may have been asked to maintain a repetitive or sustained awkward posture.
These conditions heighten the risk of getting an MSD. But factors that increase someone’s likelihood of developing MSDs are not just specific to what a boss asks you to do. The ways individuals choose to approach work and how they enjoy their time off can also contribute to the development of MSDs.

Individual-Related Risk Factor
Though we often think of MSDs as involving stressors that jobs force people to suffer, factors specific to individuals can also impact their likelihood of developing MSDs. These factors are called individual-risk factors, and they break down into four categories:
- Poor work practices — When we talk about poor work practices, we aren’t referencing the conditions people suffer because of the demands put upon them by their employers: that would be a
work-related risk factor. Rather, we’re referencing the individual decisions people make on the job that negatively affect their joint health. For instance, some people might decide to forgo lifting equipment and instead “do it the old fashion way” by carrying heavy objects without assistance. That is a poor work practice that may result in an MSD.
- Poor overall health habits — People who drink, eat, or smoke excessively are at a greater risk than most for developing MSDs.
- Poor rest and recovery — People who don’t give their bodies the time to rest and recover after strenuous work are at a greater risk than most for developing MSDs.
- Poor nutrition, hydration, and fitness —Malnourished or dehydrated people are at-risk for getting an MSD or other severe health problems.
Now that we understand what MSDs are and how people develop them, we can turn our attention to how MRIs can help diagnose musculoskeletal disorders.
How MRIs Can Help Diagnose Musculoskeletal Disorders
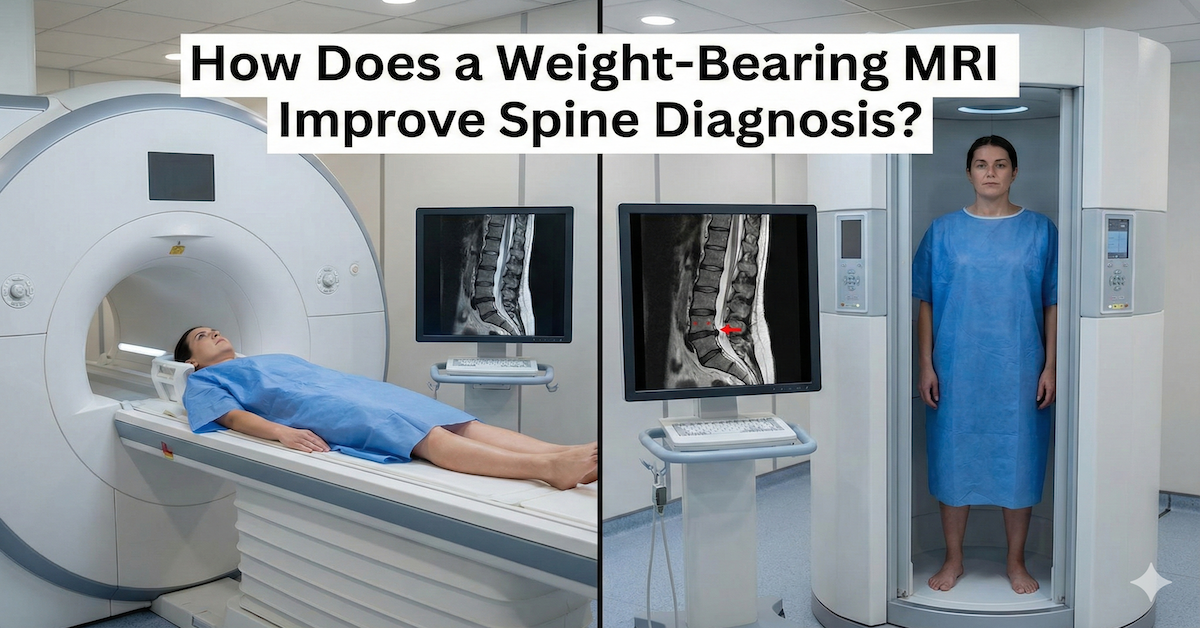
Magnetic resonance imaging, or MRI, is the perfect technique for diagnosing MSDs. MRIs use a magnetic field and radio waves to create a picture of what’s under a person’s skin. They produce pictures that are much more detailed than most imaging methods.
MRIs can examine soft tissue problems like a ruptured ligament or tendon. They can see a shoulder’s rotator cuff injury, as well as hip fractures or spinal disc abnormalities. We typically see MRIs used when diagnosing MSDs because they are especially good at detecting the following:
- Sports injuries that develop after repeated motion.
- Work injuries that develop after repeated motion.
- Tissue swelling and bleeding around joints.
- Trauma to the spinal cord.
Working with a radiologist, a doctor that specializes in interpreting medical images, patients suffering from MSDs can gain a better understanding of what’s going on in their bodies. When doctors and patients have that information, they create treatment plans to address the problem.
How MRIs Help With Treatment
After doctors discover the MSD with an MRI, they will begin applying the treatment. Treatment methods vary based on the severity of the condition and the overall health of the patient. But just because the patient has a diagnosis doesn’t mean the MRI is put away for good. Often, doctors will continue to give the patient MRIs so that they can track the progress of the person’s body. Hopefully, they will see improvements over time.
SHARE THIS POST:
Leave a Comment:
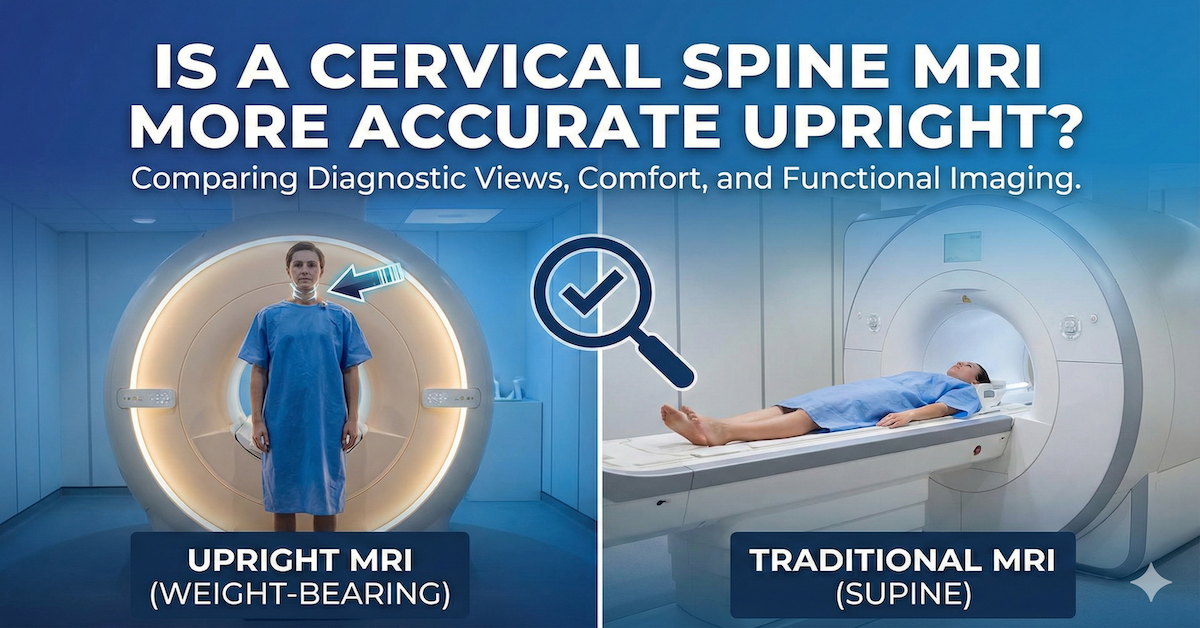
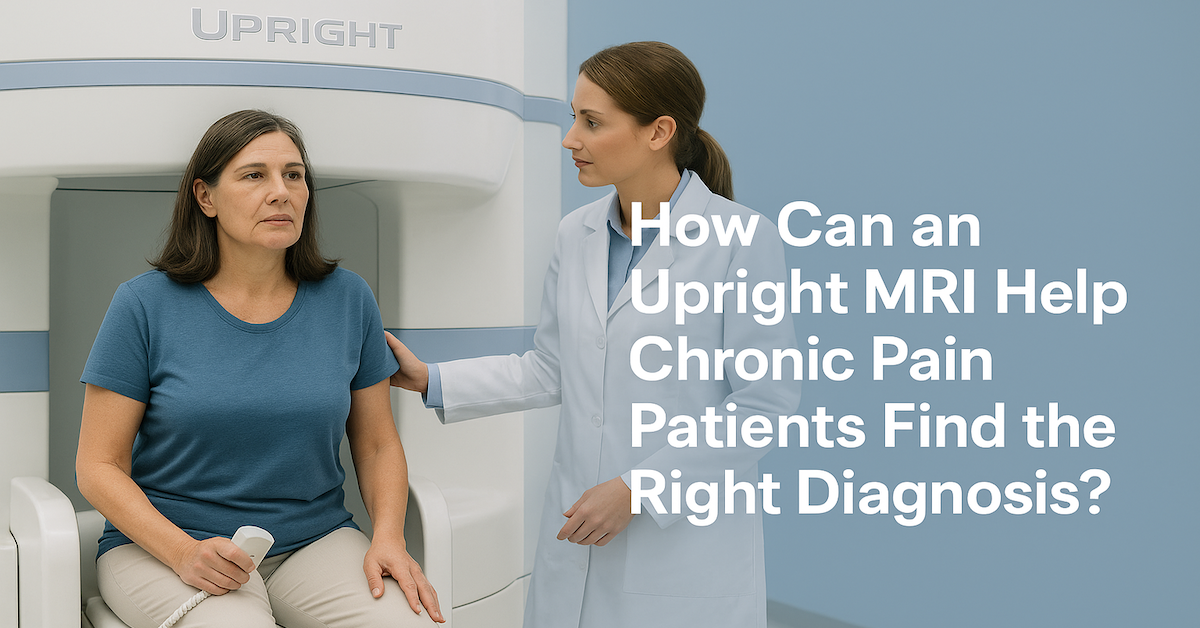
The World's Most Patient-Friendly MRI. A comfortable, stress-free, and completely reliable MRI scan. We offer patients an open, upright, standup MRI experience that helps those who are claustrophobic and stress being in a confined area. Upright MRI of Deerfield is recognized as the world leader in open MRI innovation,
Our Recent Post


READ PATIENT TESTIMONIALS
Upright MRI of Deerfield.
Susan D.,
Highland Park, 39
I am going to tell everyone about your office! This was a great experience after I panicked in other MRI machines and had to leave. Thank you so much.

Judith B.,
Milwaukee, 61
I suffer from vertigo and other MRIs do not work. This was wonderful…absolutely NO discomfort at all. The MRI was so fast…I wanted to stay and watch the movie! Mumtaz was great. His humor really put me at ease. I’ve already recommended Upright MRI to friends.

Delores P.,
Glencoe, 55
Everything is so nice and professional with your place. I have been there a couple of times. My husband and I would not go anywhere else.